Osteochondrosis does not cause pain, but at the same time pain with osteochondrosis is possible. A strange situation, at first glance. But after reading this article you will become a real expert not only on this topic, but also on: what is osteochondrosis? What are the reasons? What are the symptoms and signs? How to diagnose osteochondrosis? What effective treatment exists? What is included in the prevention of this disease? And also on many other issues.
What is osteochondrosis?
To understand what osteochondrosis is, you need to dive a little into history. The term was introduced in 1928 by Christian Georg Schmorl. But the curious thing is that Schmorl was a pathologist and, as you understand, he had no one to ask: "Where does it hurt? " (Sorry for the black humor). During his studies of pathological material, Schmorl discovered previously unknown changes in the junction between bone and cartilage, particularly in the area of the spinal discs. After describing these changes, all that remained was to find a name for them. To do this, he took the Latin word "bone" / os and the Greek word "cartilage" / chondros and, combining them, he received the term osteochondrosis.
What is osteochondrosis, as Schmorl exactly called this word? It turns out that this is not pain at all and, in general, not a sensation. With the word osteochondrosis Schmorl designated the following three changes:
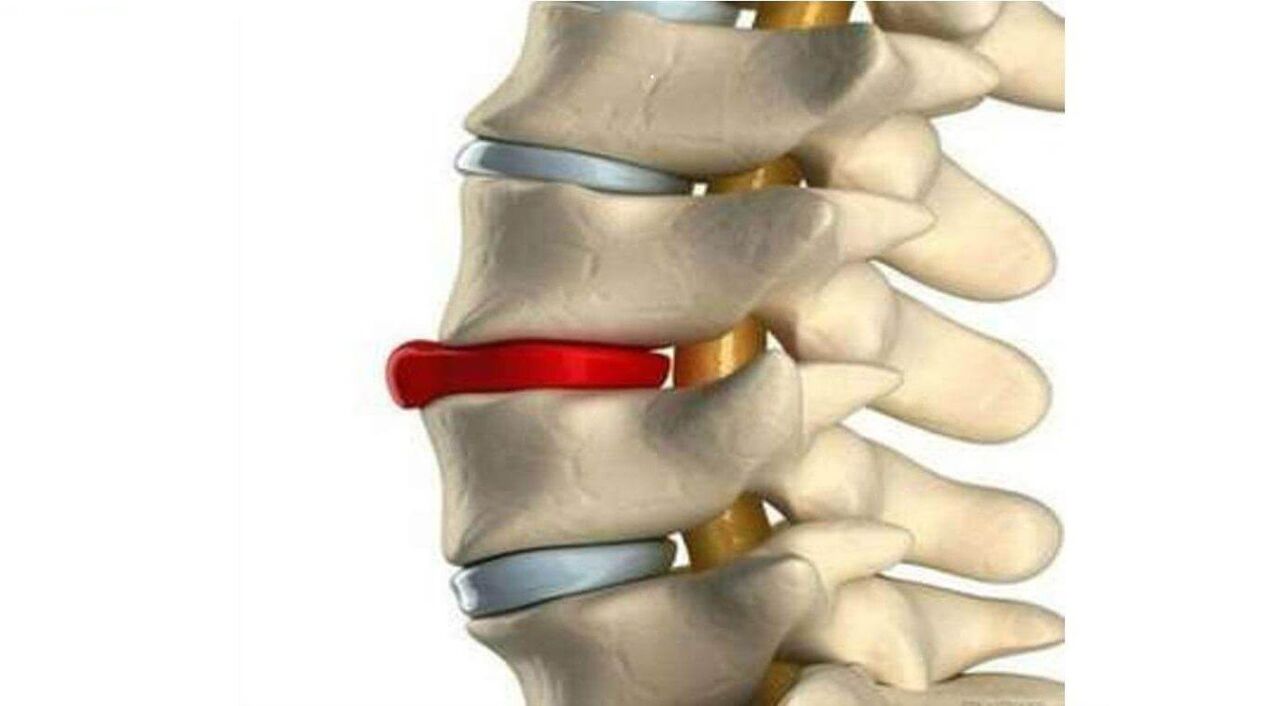
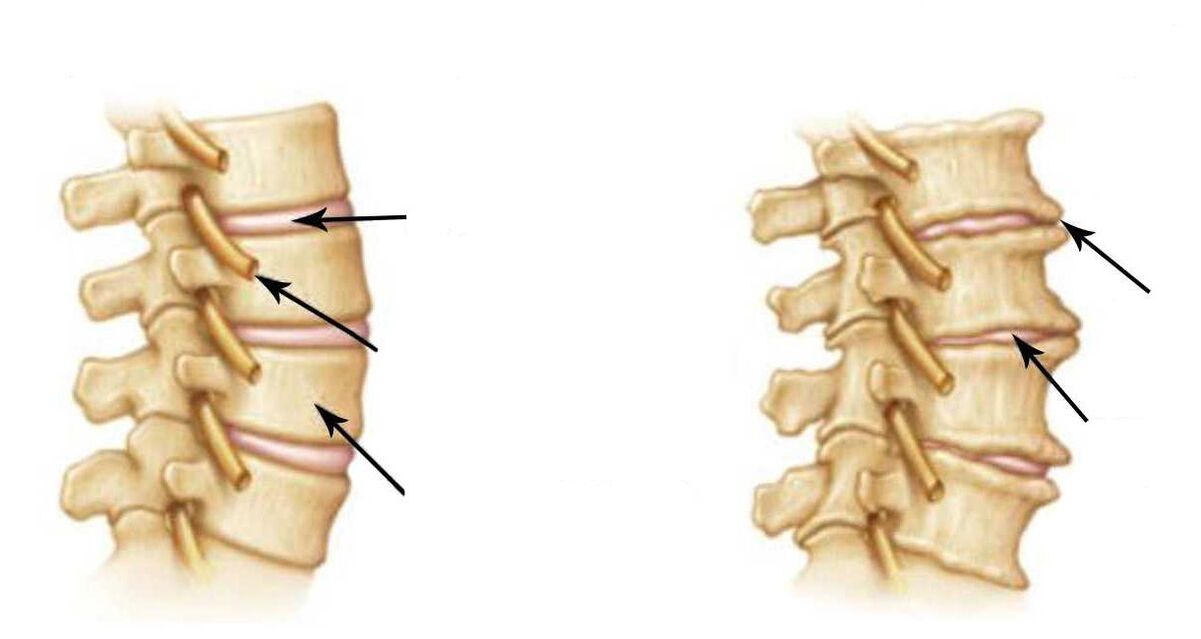
- decrease in the height of the intervertebral disc;
- subchondral sclerosis;
- marginal bony growths.
Translated into common language, this means that the height of the disc has decreased, and the surface of the vertebra adjacent to the disc has become denser and grown in the form of a rim. This is what osteochondrosis is in its original meaning, which Christian Georg Schmorl attributed to it.
Disease osteochondrosis

Let us once again pay attention to the fact that Schmorl did not describe the disease of osteochondrosis, but only tissue changes, and these are different things. The concept of "disease" is much broader and includes disorders, symptoms, laboratory and radiological changes, methods of treatment and prevention.
But Schmorl wrote nothing of the sort and, in general, did not consider osteochondrosis a disease. But then why is it customary to say that osteochondrosis is a disease, to be interested in the causes of its occurrence, its signs, symptoms and the treatment of osteochondrosis?
But the fact is that Schmorl had followers. So they decided to find out how osteochondrosis manifests itself and what symptoms bother a person? As a result, it turned out that osteochondrosis itself does not directly cause pain, as well as other sensations. This was explained by the fact that there are no pain receptors in the vertebrae and discs. And since there are no receptors, there can be no pain. This is easy to understand using the example of hair and nails: there are also no receptors or pain when they are cut.
The second important discovery was that osteochondrosis is part of a general degenerative process that involves all our organs and tissues. Dystrophy is a violation of tissue nutrition at the cellular level; it lasts for a lifetime and gradually ages our body. That is, osteochondrosis is essentially part of the aging process. But, as you know, details matter. And the detail is that not all degenerative processes are as painless as osteochondrosis. In particular, dystrophic pathology of the muscles surrounding the spine is almost always associated with pain. After all, muscles, unlike vertebrae and discs, have pain receptors. A typical example is myofascial syndrome. It usually occurs in parallel with osteochondrosis and is painful. Now, remember, at the beginning of the article we said that osteochondrosis itself does not cause pain, but is pain possible? Therefore, it is precisely these cases, when the painful pathology - the myofascial syndrome itself - is added to the painless osteochondrosis that perfectly explains the meaning of what has been said.

You may ask yourself, where is the answer to the question, why is it customary to say that osteochondrosis is a disease? Well, we're actually already getting close. The fact is that, although osteochondrosis itself is not, in fact, a disease, but being the starting point in the study of degenerative processes, the word "osteochondrosis" has taken root in our language so much that, over time, it is has become a slang name that generalizes all diseases of the spine.
Causes of osteochondrosis
The reasons can be divided into external and internal.
Internal (endogenous) causes include, first of all, the degenerative process we discussed above. This also includes genetic predisposition, as well as hormonal, mineral, vitamin, protein and other metabolic disorders, due to which the bone and cartilage tissue does not receive the necessary nutrition. All these are so-called biological factors, which, of course, can be influenced, but doing so is quite difficult and expensive. Despite this, there are simple and economical solutions that allow you to obtain no less convincing results by eliminating only the external causes.
External (exogenous) reasons are considered to be a sedentary lifestyle, poor training of the muscles of the spinal corset, microtraumas of the back and spine, insufficient physical activity, habit of bending over, "sedentary" work, constant stressful situations, lack of visits preventive measures at a chiropractor and much more.
As you can see, the external reasons are largely due to our wrong actions, for example, low physical activity, or our inertia and negligence towards our health, for example, ignoring prevention.
Agree, external causes are much easier to eliminate than internal ones. Of course, there are patients who cannot do without drug treatment for internal causes, but there are only a few of them. In most cases it is sufficient to eliminate the external causes of osteochondrosis to obtain convincing results at lower costs. This will require some self-discipline, basic physical activity, and periodic visits to a chiropractor.
Symptoms and signs of osteochondrosis
Symptoms and signs are usually divided into those that develop within the spine itself and those that are extravertebral in nature.
What do you think are the symptoms of osteochondrosis that cause the most problems? Indeed, much here depends not only on the symptoms themselves, but also on other factors: age, weight, presence of concomitant diseases in the patient, etc.
But let's go back to the symptoms of vertebral osteochondrosis: as we said they are vertebral, they are also called vertebral and extravertebral - extravertebral. Extravertebral symptoms, in turn, are also divided into two groups: reflex and radicular symptoms of osteochondrosis.
For simplicity, this classification of back symptoms is best represented as follows:
- Vertebrates/vertebral
- Extravertebral/extravertebral: radicular symptoms and reflex symptoms
Spinal symptoms of osteochondrosis include curvature of the spine (not to be confused with scoliosis), local pain, muscle tension and reduced mobility.
Radicular symptoms occur due to effects on the nerves exiting the spine. This is manifested by decreased reflexes, muscle weakness, reduced sensitivity and radicular pain.
And here it is necessary to explain that all our vertebrae, discs and "roots" have a certain designation. Therefore, we can talk about radicular symptoms only when all these symptoms and signs clearly indicate a specific "root", and not when any "bulldozer" pain is called radicular.
Very rare but dangerous signs and symptoms of osteochondrosis are paresis, paralysis and destruction of the pelvic organs. They indicate the development of a spinal stroke. This is a serious complication of osteochondrosis, in which the radicular arteries are affected.
Reflex symptoms mainly depend on which part of the spine is affected. According to statistics, the cervical spine is most often affected.
The essence of cervical osteochondrosis is a large number of reflex symptoms. Pain in the neck, back of the head and collar area. Creaking of the vertebrae, muscle tension and difficulty in movement. Heachache. Dizziness. Intracranial pressure. Morning stiffness. Numbness, tingling, goosebumps and weakness in the arms. Pain in the shoulders and under the shoulder blade. Burning between the shoulder blades and in the heart area (reminiscent of angina). Numbness in the hands or fingers. "Swelling" in the area of the seventh cervical vertebra. Temporary darkening or "floaters" in the eyes. Noise or ringing in the ears. Nausea, even vomiting. Pressure spikes. Pre-fainting state. A lump in the throat with osteochondrosis, weakening of the voice, hoarseness, feeling of lack of air, problems swallowing and sore throat with osteochondrosis - all these are quite common reflex symptoms. Sleep disturbances, frequent insomnia and feeling tired in the morning may also occur. General weakness. Irritability. Rapid fatigue.
As you can see, the symptoms and signs of the disease with osteochondrosis are very diverse. This is especially true for reflex symptoms.
Diagnosis of osteochondrosis
Diagnosis is the key to appropriate treatment. Modern hardware diagnostic methods allow you to accurately confirm this diagnosis. As you know, MRI and CT are considered the most accurate tests. But, as before, the main factor in diagnosis remains the clinical diagnosis. This happens when an expert doctor compares data from at least three sources: the patient's complaints, the MRI results, and the symptoms identified during the exam.
This approach to diagnostics allows you to establish an accurate diagnosis and develop an individual effective treatment program.
Effective treatment of osteochondrosis
Effective treatment of osteochondrosis is possible only with strict adherence to a scientific approach. This means that correct prioritization is necessary, first of all, when choosing the main and auxiliary types of treatment for vertebral osteochondrosis.
What do you think is the most important treatment? You don't need to be a doctor to answer this question. You can just follow the logic. Osteochondrosis is a pathology of the musculoskeletal system. This system is biomechanical in nature. The key word is "mechanical". Accordingly, mechanical disorders require the same treatment methods – mechanical. Therefore, the main type of treatment for osteochondrosis is manual therapy. It is ideal for restoring the biomechanics of the musculoskeletal system. And auxiliary methods include medications, physiotherapy, massage, physical therapy, etc. And it is also important to know that among all types of manual treatment, the safest type is gentle manual therapy. It is superior to conventional manual therapy in terms of effectiveness, gentleness and safety. To understand what the treatment of osteochondrosis by a chiropractor consists of, it is necessary to know that the intervertebral discs are the only part of the body that does not have blood vessels and is nourished thanks to the correct functioning of the spinal muscles. The failure of these muscles to function immediately compromises the nutrition of the discs. And as we said at the beginning of the article, malnutrition is precisely the degenerative process of which osteochondrosis is part.
Effective treatment with gentle manual therapy is fundamentally different from conventional manual therapy. This is not a "vertebral realignment" at all, as some think: it is something completely different. Gentle manual therapy is a whole system of special methods of influence that eliminate muscle spasms and tension. It brings the muscles back to their normal physiology and improves the nutrition of the discs.
Observation by a doctor includes three stages:
- Consultation. The doctor finds out what symptoms bother the patient, clarifies the medical history, studies the patient's medical documentation, analyzes the images and determines the nature of the disease.
- Diagnostics. Conducts a thorough examination and clinical examination of the patient: visual and myofascial diagnostics; palpation of tense muscles and painful vertebrae; neurological reflex tests and muscle tests.
- Treatment plan. Based on the history of the current disease, examination data and the results of the patient's clinical examination, the doctor formulates a diagnosis and selects treatment options. The doctor tells the patient in detail about the essence of the disease and the principles of treatment and answers all the patient's questions.
Prevention of osteochondrosis
Prevention is necessary to avoid relapses. To do this, it is necessary to create comfortable conditions for work and rest. Maintain physical activity. Avoid overwork. Monitor proper nutrition and weight. But the main thing is not to neglect your health.
Remember, prevention is, first of all, medical control and timely correction of the musculoskeletal system. Try to visit a chiropractor at least once every three to six months. This will reduce risk factors and eliminate any breaches in a timely manner. Advanced osteochondrosis leads to complications: disc protrusions and herniations. Do not forget. Take care of yourself!



















